This month, the Office of Graduate Medical Education is celebrating its second class of Quality Improvement and Patient Safety (QIPS) Certificate Program graduates. A small cohort of residents and fellows spent the past academic year growing in quality improvement and patient safety. They also conducted a QI capstone project and had the opportunity to present at the Quality Improvement and Patient Safety Poster Forum on May 21.
Among the posters presented was one by emergency medicine resident, Madeline Haase, MD, focused on evaluating the accuracy of physicians working in the physician-in-triage (PIT) system in the emergency department. Her project asked two key questions: how accurate are providers at predicting whether a patient will be admitted, and how long do they expect a patient to remain in the ER?
“As an ER resident, the PIT system really helps with streamlining patient care and handling lower-acuity patients,” said Dr. Haase. “It was beneficial to see how accurate physicians were at predicting admissions and patient length of stay, which can help with planning in the ER and also for admitting services.”
For Mallory Vaughn, MD, her QI project tackled the challenge of lengthy hospital stays for patients with chest pain, particularly those considered low to intermediate risk. An alumna of the UK College of Medicine-Bowling Green Campus, Dr. Vaughn is now an internal medicine resident in Bowling Green. She discovered that her rural hospital had an average patient stay of nearly 50 hours, compared to a national average of 16 to 24 hours. “I wanted to figure out why we were seeing such a large discrepancy at our location,” said Dr. Vaughn.
Her project emphasized improving guideline-based screening both in the emergency department and by primary admitting teams. More than a matter of efficiency, Dr. Vaughn emphasized the connection to patient-centered care. “The main question I get asked pretty much every time I admit a patient is, ‘when can I go home?’” she said. “These are days where patients can’t work or take care of their children,” she noted. “We want to give good, effective health care, but do so in a way that’s conscientious of the patient and their life.”
These examples showcase the power of collaboration and reflective practice in improving patient outcomes. As these residents and fellows continue their training, their projects serve as foundations for lasting improvement and real change in how care is delivered.
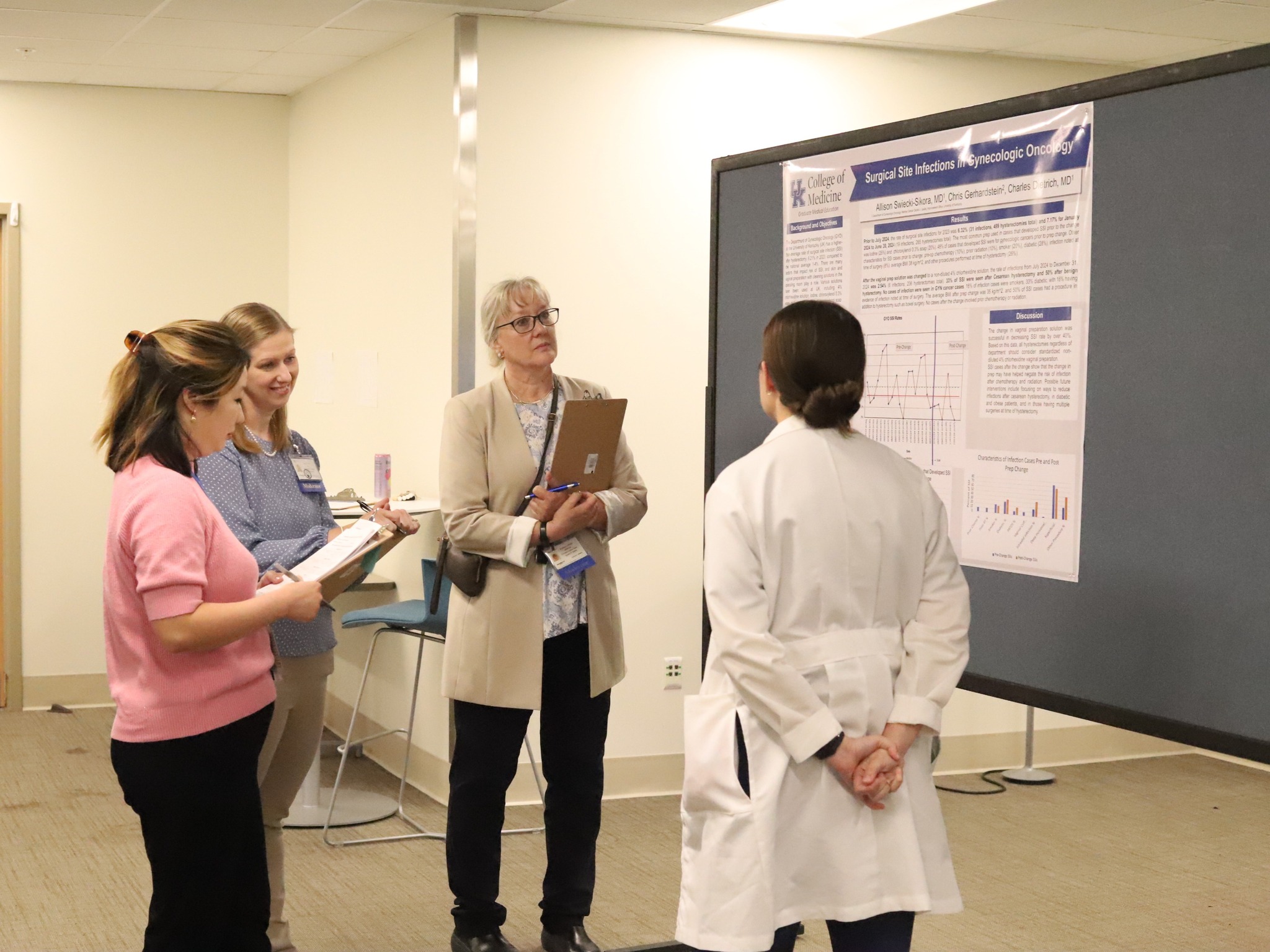
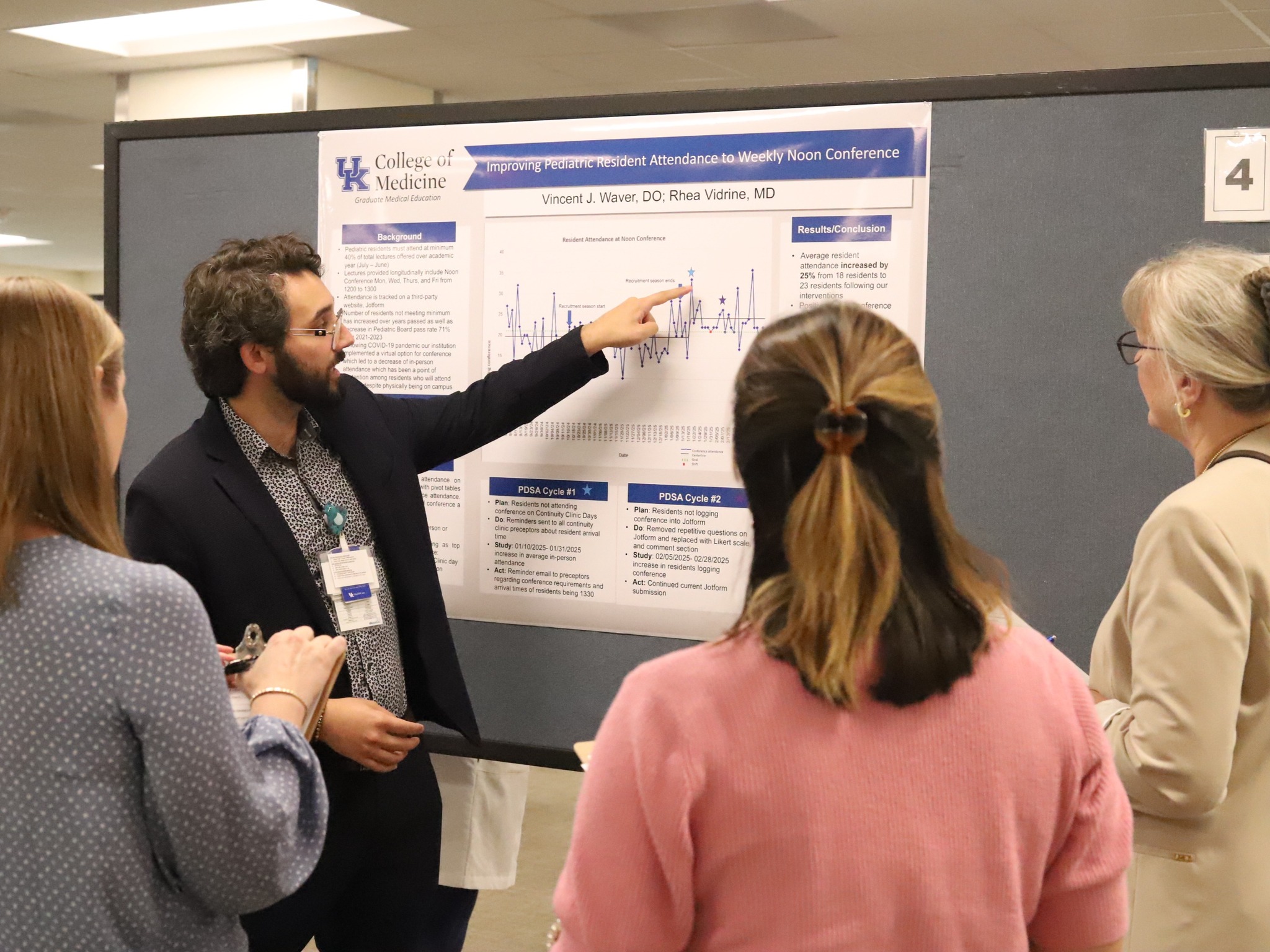
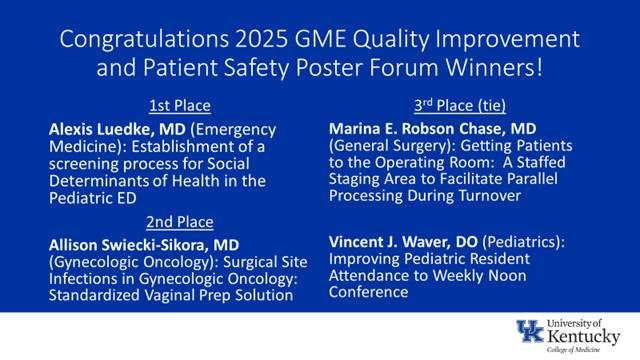
The QIPS poster forum was organized by the Office of Graduate Medical Education, and projects were judged by a group of hospital leaders, program directors, faculty, and residents. Thanks go out to all of the presenters and their colleagues and faculty mentors who worked on these efforts to improve quality, safety, and efficiency in their respective specialties, as well as UK HealthCare as a whole. Special congratulations to the project winners listed below!
1st Place:
Alexis Luedke, MD, (Emergency Medicine)
“Establishment of a Screening Process for Social Determinants of Health in the Pediatric ED”
2nd Place:
Allison Swiecki-Sikora, MD, (Gynecologic Oncology)
“Surgical Site Infections in Gynecologic Oncology Standardized Vaginal Prep Solution”
3rd Place (tie):
Marina Robson Chase, MD, (General Surgery)
“Getting Patients to the Operating Room: A Staffed Staging Area to Facilitate Parallel Processing During Turnover”
Vincent J. Waver, DO, (Pediatrics)
“Improving Pediatric Resident Attendance to Weekly Noon Conference”
Congratulations to the 2024-2025 QIPS Certificate Program Graduates:
David Carter, MD (Internal Medicine)
Amanda Henderson, MD (Pediatrics)
Allison Swiecki-Sikora, MD (Gynecologic Oncology)
Mallory Vaughn, MD, MBA (Internal Medicine, Bowling Green Campus)
Vincent Waver, DO (Pediatrics, Chief Resident)