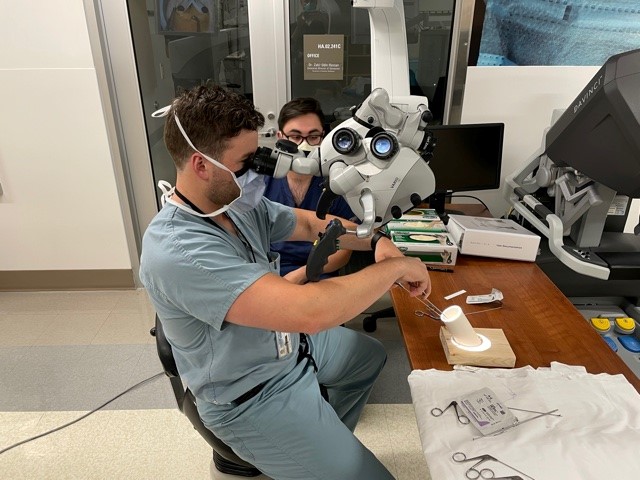
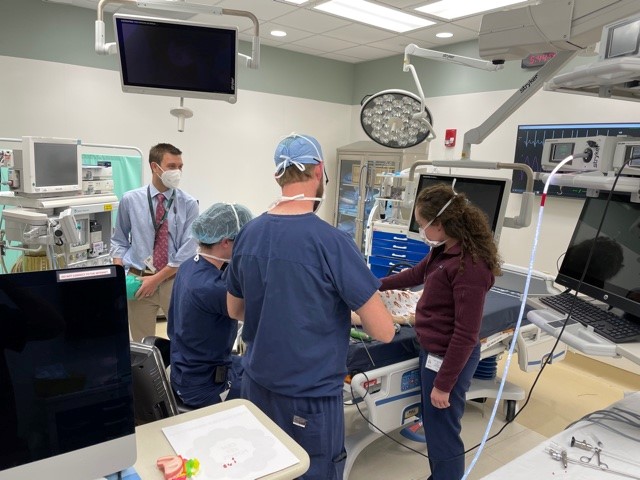
Simulation
UK otolaryngology believes that the best way to learn surgery or clinical procedures is to be actively involved, virtually always on a one-on-one basis with an attending physician. However, there are certainly times when simulation can enhance resident and student learning, and we embrace using simulation scenarios. Specifically, we attempt to have one “wet lab” simulation with every resident teaching series (RTS) topic, as well as other simulations throughout the year. For example, UK otolaryngology has a temporal bone course with neurotology teaching. UK otolaryngology also has a sinus dissection course with the rhinology RTS, allergy injection training with the allergy RTS, maxillofacial plating with the facial plastics and reconstructive surgery RTS, and pediatric airway foreign body removal with the pediatric otolaryngology RTS.