Recent Faculty Publication: Cathelicidin Related Antimicrobial Peptide (CRAMP) Enhances Bone Marrow Cell Retention and Attenuates Cardiac Dysfunction in a Mouse Model of Myocardial Infarction
Yuri M. Klyachkin, Amr Idris, Christopher B. Rodell, Himi Tripathi, Shaojing Ye, Prabha Nagareddy, Ahmed Asfour, Erhe Gao, Rahul Annabathula, Mariusz Ratajczak, Jason A. Burdick, Ahmed Abdel-Latif*
Abstract
Background
Acute myocardial infarction (MI) and the ensuing ischemic heart disease are approaching epidemic state. Unfortunately, no definitive therapies are available and human regenerative therapies have conflicting results. Limited stem cell retention following intracoronary administration has reduced the clinical efficacy of this novel therapy. Cathelicidin related antimicrobial peptides (CRAMPs) enhance chemotactic responsiveness of BMSPCs to low SDF-1 gradients, suggesting a potential role in BMSPCs engraftment. Here, we assessed the therapeutic efficacy of CRAMPs in the context of BMSPCs recruitment and retention via intracardiac delivery of CRAMP-treated BMSPCs or CRAMP-releasing hydrogels (HG) post-AMI.
Methods
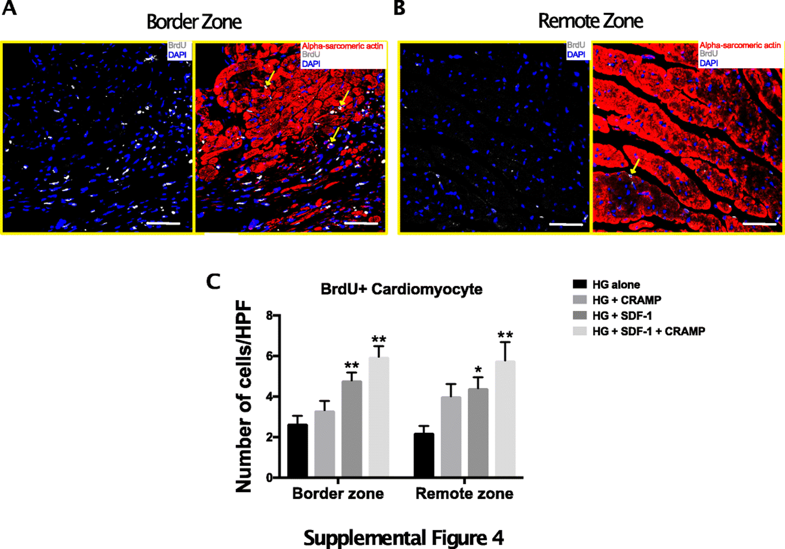
For cell transplantation experiments, mice were randomized into 3 groups: MI followed by injection of PBS, BMMNCs alone, and BMMNCs pre-incubated with CRAMP. During the in vivo HG studies, BM GFP chimera mice were randomized into 4 groups: MI followed by injection of HG alone, HG + SDF-1, HG + CRAMP, HG + SDF-1 + CRAMP. Changes in cardiac function at 5 weeks after MI were assessed using echocardiography. Angiogenesis was assessed using isolectin staining for capillary density.
Results
Mice treated with BMMNCs pre-incubated with CRAMP had smaller scars, enhanced cardiac recovery and less adverse remodeling. Histologically, this group had higher capillary density. Similarly, sustained CRAMP release from hydrogels enhanced the therapeutic effect of SDF-1, leading to enhanced functional recovery, smaller scar size and higher capillary density.
Conclusion
Cathelicidins enhance BMMNC retention and recruitment after intramyocardial administration post-AMI resulting in improvements in heart physiology and recovery. Therapies employing these strategies may represent an attractive method for improving outcomes of regenerative therapies in human studies.
Link to article and supplementary materials
*Saha Cardiovascular Research Center