We are pleased to share a POV with you this week from UKEM alumnus and USAF Major, Dr. Chris Belcher. Dr. Belcher completed his residency at UK in 2018 and is currently based out of Texas.
**Views expressed are solely the author's and don’t represent the Department of Defense, the United States Air Force, or the San Antonio Uniformed Services Health Education Consortium**
“This is beautiful scenery but why are we circling so many times?” I asked the C-17 pilots circling the flight line on our way to pick up a critically ill patient in a warzone in the Middle East.
“Oh, we’re just waiting for them to stop launching mortars.” Co-pilot.
“Cool...cool...cool.” - Me, not going to ask anymore questions.
Afterwards, I told my wife about this from the safety of Germany. After a successful mission delivering the patients and thinking how close I was to the end of my deployment, I thought it would make for a good story. In retrospect, that was a poor life choice. Given our deployment was extended some bonus months (thanks COVID) and we’d be sent out on more missions, this did not help her worries. Thankfully we can now look back at this and laugh at my poor judgement from the safety of our home on American soil. Air Force Emergency Medicine physicians lead double lives. Back home in the states, we work in Emergency departments just like our civilian counterparts. We mostly take care of the active duty and retiree population. But when we deploy, we have a multitude of jobs that we can be tasked to perform--ground surgical team members working closer to the wars’ frontlines, emergency medicine physicians at the more well established medical treatment facilities, or critical care transport specialists flying wounded and critically ill service members between levels of care.
When I’m stateside, I work at Brooke Army Medical Center--the DOD’s only level I trauma center, burn center, and an academic quaternary referral center. We mostly take care of the active duty and retiree population but also have a unique role in managing civilian trauma and burns. I work closely with the residents and am currently serving as one of the Assistant Program Directors for our residency. I am also on call for the critical care air transport teams (CCATT) that are utilized for transfer of service members stateside or occasionally in natural disasters. I was also trained for our unique ECMO cannulation and transfer team prior to my deployment.
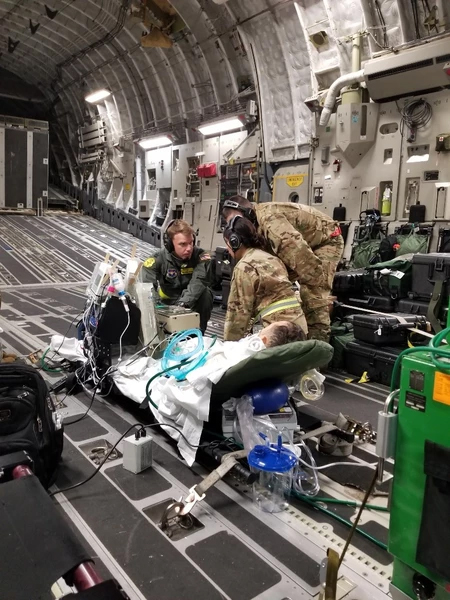
My deployment mission involves being the ICU in the sky. With a team of myself, a critical care nurse, and a respiratory therapist, we are tasked to transport critically ill patients to higher levels of care. While deployed during 2019-2020, many of these missions involved delivering patients from war zone facilities in the middle east to the safety of Germany and a quaternary care hospital. We utilized C-130 and C-17 airplanes to deliver ICU level care during transport. Low light, super loud planes, altitude, limited diagnostics and treatment options, and logistical conundrums makes for unique and challenging medical care.
My training at the University of Kentucky helped lay the foundation for the medical knowledge and clinical flexibility that is needed to perform my job(s). I was exposed to a high volume of patients with high acuity and had great mentors that helped create a solid medical knowledge base. I was also given the opportunity to manage a large amount of critically ill patients for extended periods. This has helped the transition to ICU level management for long flights in less than ideal conditions. I am very thankful for the training that was provided to me in medical school and residency at UK.
As I begin my transition away from active duty military life back to the civilian world, I am thankful for the opportunities that Air Force medicine gave me. I was able to perform unique jobs and take care of a great patient population. My training at the University of Kentucky Department of Emergency Medicine helped lay the groundwork to deliver great patient care during my active duty time.