After years of virtual meetings and long-distance conversation, faculty members from the UK College of Medicine Department of Surgery were finally able to meet face-to-face with colleagues from the University Teaching Hospital (UTH) in Lusaka, Zambia last January as part of the American College of Surgeons’ Health Outreach Program for Equity in Global Surgery (ACS H.O.P.E.).
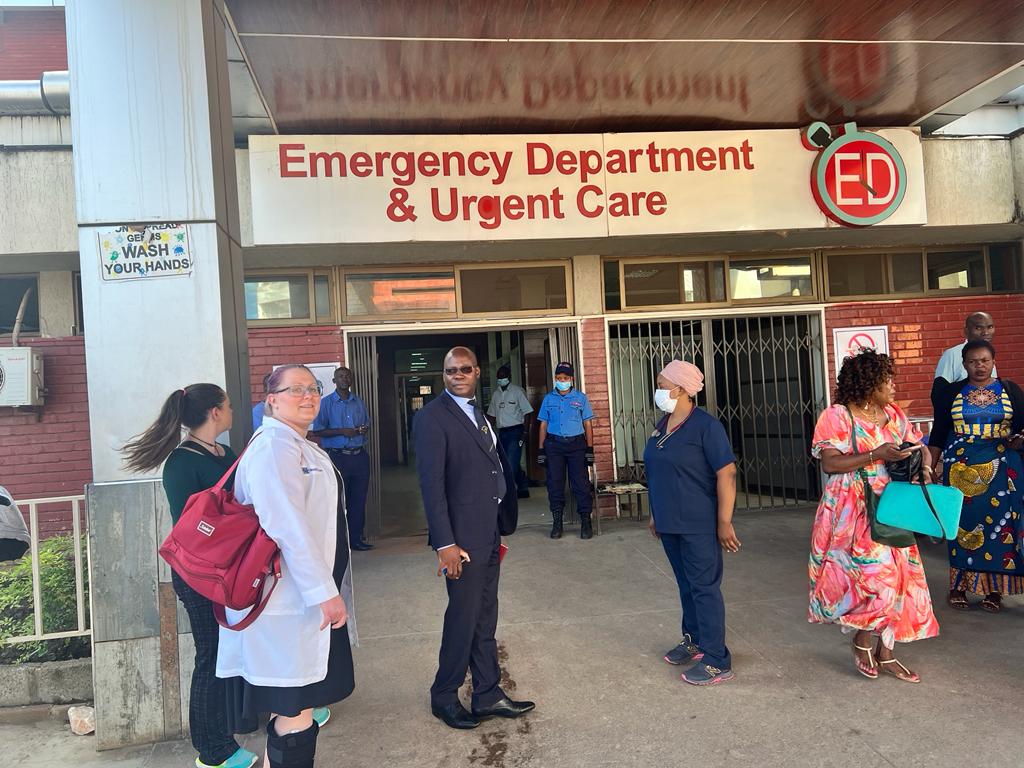
Alexis Nickols, MD, and Brittany Wheelock, MD, from the division of trauma and critical care surgery, joined Dr. William B. Inabnet III, the Johnston-Wright Endowed Professor and chair of surgery, for a two-week visit with faculty and residents at Zambia’s largest teaching hospital.
The department of surgery is a member of the Lusaka Surgical Training Collaborative, established in 2019 by the ACS H.O.P.E. program. The Lusaka Collaborative is a partnership between UTH, composed of five different hospitals in the capital city, and about a dozen ACS-member Departments of Surgery in the United States.
The collaborative is intended as an opportunity for surgeons on both continents to share knowledge through their unique experiences in patient care and surgical education. Plans for on-site visits between collaborative participants in the last three years were hampered by the lasting effects of the COVID-19 pandemic. Some official visits from collaborative partners began around 2022, but most activities remained virtual. UK Surgery maintained an open invitation for UTH faculty and residents to access grand rounds and M&M.
Virtual meetings did allow the collaborative to conduct a needs assessment in which specific goals for UTH were identified. Among those needs was a desire to implement a formal quality improvement program aimed at surgical outcomes and assistance in mentoring UTH surgery residents in advanced techniques in minimally invasive surgery.
Dr. Nickols heads the collaborative’s Quality Improvement initiative. The objective for this first on-site visit, she explained, was to establish relationships with UTH colleagues who would be involved in the program’s development.
“We had a lot of good conversations about the type of records-keeping and reporting needed for quality improvement,” Dr. Nickols said. The committee identified barriers to be addressed in the coming year for the process to move forward.
Drs. Wheelock and Nickols also conducted a critical care needs assessment. Together with UTH providers in the critical care response team, several opportunities for improvement were identified.
Despite the difference in geography, the issues facing critical care teams at UK and UTH are very similar. “We face many of the same challenges and frustrations,” Dr. Nickols observed.
Another benefit of visiting UTH in person, Drs. Nickols, Wheelock, and Inabnet spent time with general surgery residents working on exercises in laparoscopic surgery fundamentals.
The most important outcome of this first overseas journey was making good contacts and building working relationships. While technology has enabled collaborative members to communicate and interact over the last three years, meeting colleagues in person makes a significant difference and demonstrates a higher level of commitment to achieving the goals of the ACS H.O.P.E. program.
As one of the members of the ACS H.O.P.E. Hub in Zambia, the UK surgery department plans to send representatives to UTH for one month each year for at least the next five years or longer. The department is also seeking approval through the Accreditation Council of Graduate Medical Education (ACGME) to approve international rotations that will allow residents to participate in the program.