
Pathology Core Curriculum
UK Pathology Core Curriculum for AP/CP Residents
Innovative, Two-Year Core Curriculum
The UK Pathology Core Curriculum (PCC) is an innovative two-year core curriculum wherein we broadly engage six strategies of adult learning to teach anatomic and clinical pathology. We interleave AP and CP topics organized by organ/organ system. Crucially, the PCC expands beyond a traditional didactic lecture series to incorporate retrieval practice (RP) in five formats. Active learning amplifies knowledge retention, and with this novel, intensive curriculum, we VIGOROUSLY engage in it and quantitatively gauge it.
Faculty, Trainees, and Staff
All residents participate. Since the cycle is two years, the resident experiences the total curriculum twice reinforcing content consolidation. For each teaching block, which roughly corresponds to an organ or organ system, AP and CP content experts provide lectures or interactive learning sessions accompanied by unknown slide conferences and CP case conferences. We assign an additional faculty member with special expertise in the PCC who acts as a consultant to the content experts who primarily facilitates creating retrieval practices. We use five RP formats (see below). Our Residency Program Coordinator and an administrative assistant provide operational support.
Rationale
According to cognitive psychology and pedagogical research, learning occurs in at least three steps: 1) encoding of information (in short term memory such as with initial reading or re-reading of a topic); 2) consolidation or reorganization and stabilization of information (transfer to long term memory); and 3) retrieval of information (ability to recall the information for real time use). Cognitive psychology studies show that “periodic retrieval of learning helps strengthen connections to the memory and the cues for recalling it, while also weakening routes to competing memories.”1 “Periodic retrieval of learning” = retrieval practice. We aim to strengthen anatomic and clinical pathology working knowledge in our residents to optimize their performance in standard testing, improve their clinical practice, and serve as a scaffold on which our residents, as practitioners, creatively continue to effectively learn in pathology, a continuously evolving and vital keystone field of medicine.
Six Strategies of Adult Learning
With the PCC, we employ the six main strategies of adult learning:
1. Spaced Practice: spreading subject materials and study activities over time
- At UK, residents experience the core curriculum twice over four years
2. Retrieval Practice: proven more effective than massed learning (cramming) and reading/re-reading
- At UK, residents augment assigned reading with content expert lectures and active learning sessions, and learning continues throughout the four years
3. Elaboration: delving further into the subject material to connect across subject areas
- At UK, the residents engage in elaborative interrogation of the materials as the core curriculum proceeds making connections across topics; for example, learning about sarcoma genetics as fusion driven or aneuploidy driven raises opportunities to explore the general tumor promoting effects of aging
4. Interleaving: switching between topics or types of problems while studying
- At UK, residents learn basic surgical pathology features of tumors but also learn corresponding microbiology, clinical chemistry or molecular aspects of the same tumors in the same block. For example: we combine diagnostic histopathology of colon cancer subtypes with an interactive learning session on microsatellite instability (MSI)-high and -low tumors.
5. Concrete Examples: illustrating abstract concepts with specific examples
- At UK, we regularly discuss pathologic entities in the setting of a case presentation
- At UK, the faculty on the anatomic pathology rotations actively query the residents when signing out daily, active clinical cases. In these sign-outs, faculty re-engage the resident in learning the block subject matter in a real-time clinical context.
6. Dual Coding: combining words with visuals to provide two pathways to retrieve information later
- At UK, the residents are referred to relevant chapters in surgical pathology textbooks for each organ or organ system block. They dual code the content they have read about visually through rapid-fire review sessions, unknown slide conference, retrieval practice quizzes, and team-based learning sessions.
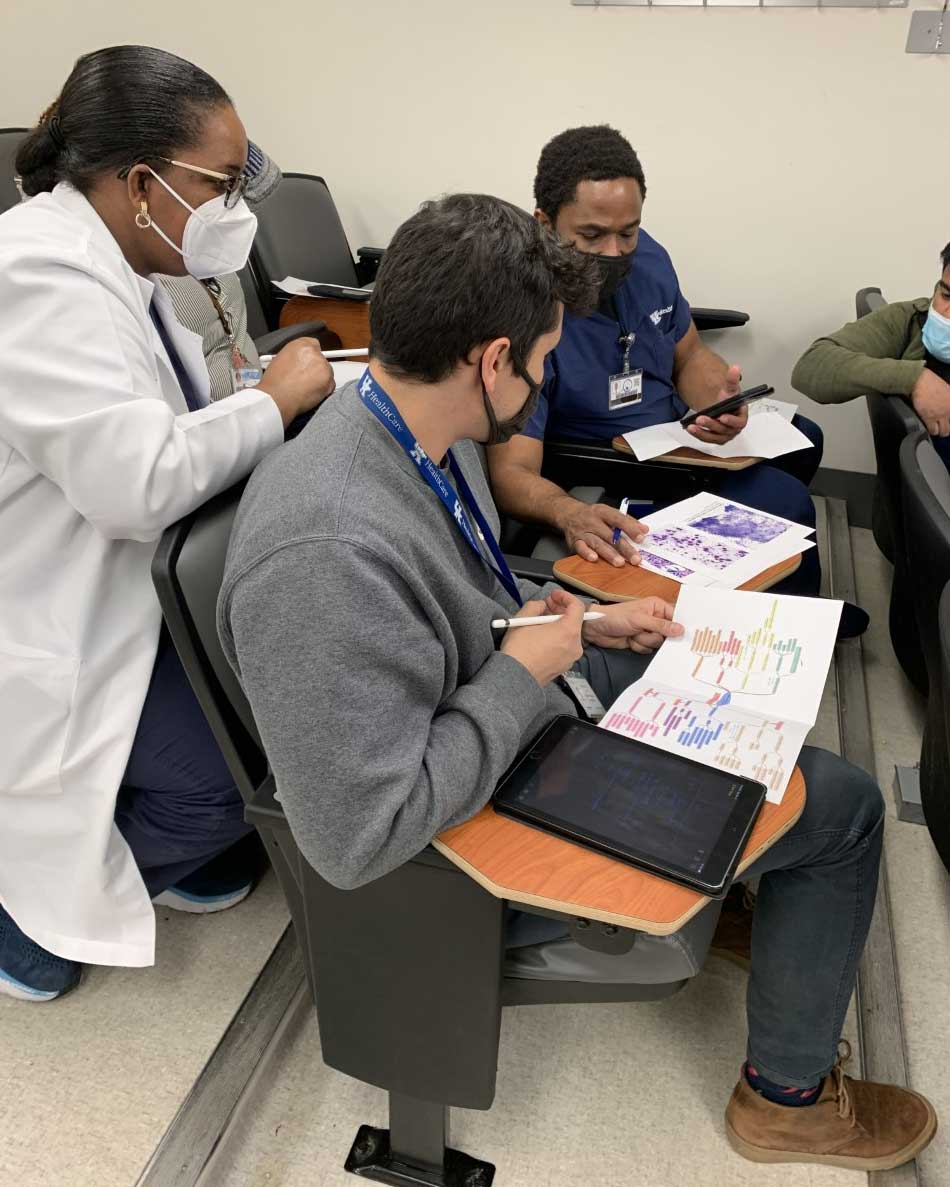
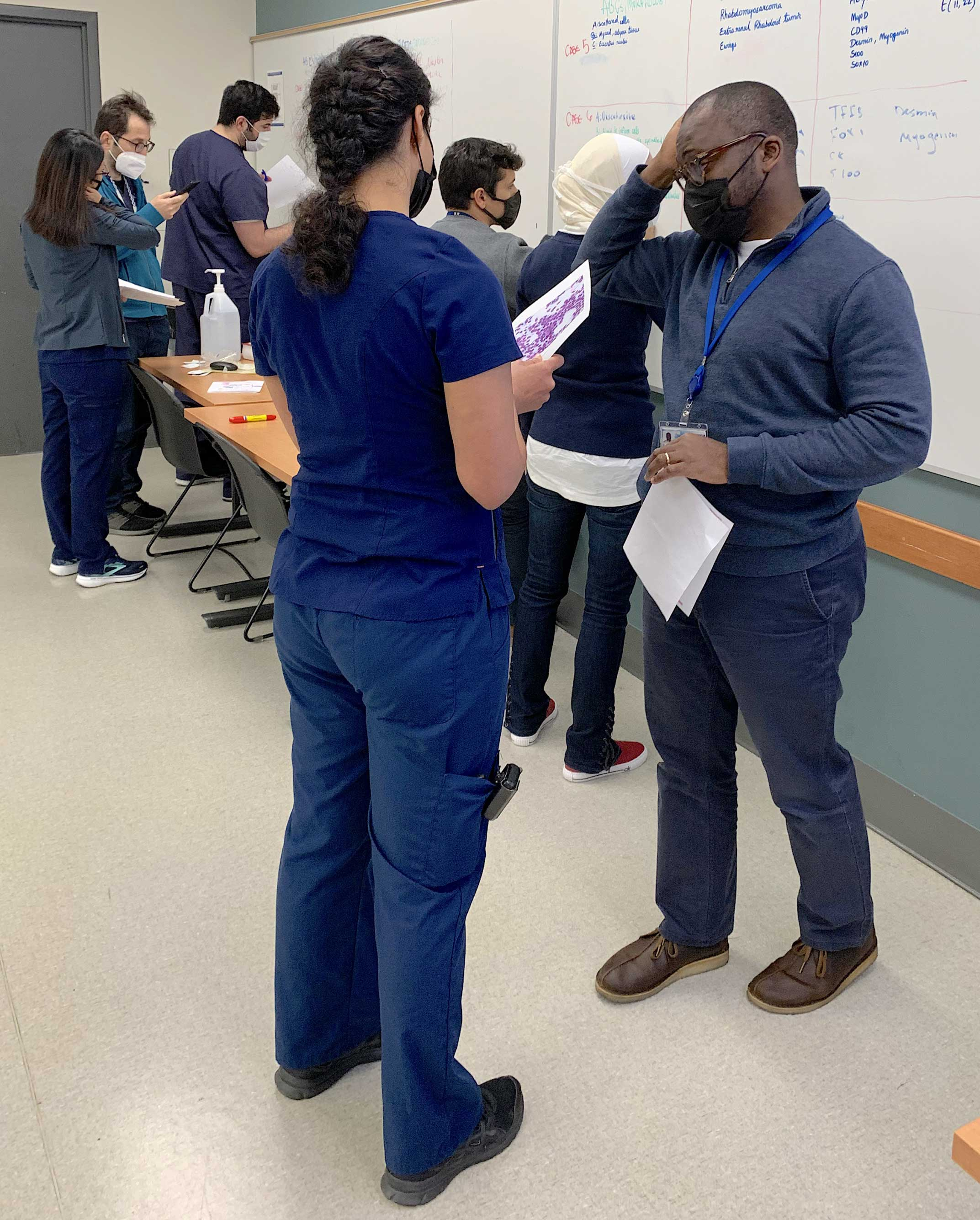
Five Formats of Active Learning (Retrieval Practices)
At UK, we employ five formats of retrieval practice in the PCC: 1) retrieval practice in the form of ExamSoftTM quizzes; 2) team-based learning in the form of Jeopardy-like sessions; 3) real time identification of pathology by rapid fire review using projected photomicrographs; 4) texting of quiz questions (with or without images); 5) and the traditional unknown slide conference.
Over the two-year curriculum, residents undergo several dozen RPs in the form of ExamSoftTM quizzes. The quizzes also include bi-annual cumulative quizzes. We publicly recognize top performers with certificates and gift cards. ExamSoftTM retrieval practices accommodate not only multiple-choice type questions but also short answer, essay, true-false, matching and identification of key histologic features in photomicrographs. To further enhance learning, the faculty member thoroughly reviews the answers to the ExamSoft RP with the residents. We schedule the review at an interval of one to four days following the retrieval practice, because evidence shows that spacing between the RP session and formal review of answers enhances retention.
Evidence Based Data Tracking
We capitalize on data aggregation strengths of the ExamSoftTM software to track individual resident performance through time and by subject matter, among assessing other metrics. We correlate RP performance with performance in anatomic pathology rotations, the RISE exams, and AP/CP Boards. We anticipate providing targeted additional training in areas identified as weak by RP performance.
Schedule
We began the Pathology Core Curriculum with the gastrointestinal tract (GIT) block covering seven organs in approximately 10 weeks. (See below for the schedule.) For the two-year cycle, we post all reading assignments and scheduled learning sessions/RPs in MicroSoft Outlook. As all faculty and trainees have UK Outlook accounts, the schedule clearly alerts faculty (and self-directed trainees) concurrent opportunities for elaborative interrogation on the topics covered in the PCC while the residents rotate through AP and CP divisions. For example, during the neuropathology block, a microbiologist can discuss the infectious causes of encephalitis and progress in diagnosing a real-time patient in greater detail with the resident rotating concurrently on microbiology. We regard this integration of the formal PCC with simultaneous rotations as 3600 learning. Three sixty degrees learning also encompasses residents educating other physicians and each other.
For an example, view a PCC schedule at the link below
Scholarly Activity
We periodically analyze the PCC program effectiveness in an evidence-based manner. Subsequently, we plan to present our results to the graduate medical education community via peer-reviewed publications. See below for our initial peer reviewed publication.2
References
-
Make It Stick: The Science of Successful Learning. Peter C. Brown, Henry L. Roediger III, Mark A McDaniel. Belknap/Harvard Press: Cambridge MA, 2014.
-
Neltner J, Bocklage T. Levering Adult Learning Principles into a Residency Core Curriculum. Cancer Cytopathology 2021 Jul;129(7):501-505. doi: 10.1002/cncy.22418. Epub 2021 Mar 19.
Education Committee Members
The education committee meets once a week to discuss ways to implement adult learning principles into their teaching and mentoring.
- Janna Neltner, MD
- Robert McDonald, DO
- Nathan Shelman, MD
- Aaron Shmookler, MD
- Robert D Maynard, PhD
- Sahar Nozad, MD
- Justin Rueckert, MD
- Thèrése Bocklage, MD
- Derek Allison, MD
- Leanna Brignola, MAed
Adult Learning Principles
Interview with Dr. Thèrése Bocklage, Vice Chair of Education in the Department of Pathology and Lab Medicine:
What does the term "Adult Learning" mean and how does it apply to the UK Pathology Residency Program?
Adult learning is a concept explored for decades and describes the differences between children and adult learning and how concepts are absorbed. At UK, we incorporate adult learning principles to maximize adult learning through our two year pathology core curriculum. Specially, we follow the Six Strategies of Learning.
How do you motivate and engage an adult learner?
To begin, our residents already arrive motivated. Then we promote active learning, including an emphasis on individual cases, and residents master the material. Through our passion for pathology, we hope our enthusiasm is contagious.
Since applying these learning principles to this residency program, what changes have you seen?
We have seen improvement in general through performance in external measures of knowledge such as the RISE exam and in personal knowledge as measured in periodic retrieval practices and clinical responsibilities.